글로벌 연구동향
방사선종양학
- [Cancer Res Treat.] Clinical Outcomes of Postoperative Radiotherapy Following Radical Prostatectomy in Patients with Localized Prostate Cancer: A Multicenter Retrospective Study (KROG 18-01) of a Korean Population.
국립암센터 / 이성욱, 조관호*
- 출처
- Cancer Res Treat.
- 등재일
- 2020 Jan
- 저널이슈번호
- 52(1):167-180. doi: 10.4143/crt.2019.126. Epub 2019 Jun 25.
- 내용
Abstract
PURPOSE:
The purpose of this study was to investigate the clinical outcomes of postoperative radiotherapy (PORT) patients who underwent radical prostatectomy for localized prostate cancer.Materials and Methods:
Localized prostate cancer patients who received PORT after radical prostatectomy between 2001 and 2012 were identified retrospectively in a multi-institutional database. In total, 1,117 patients in 19 institutions were included. Biochemical failure after PORT was defined as prostate-specific antigen (PSA) ≥ nadir+2 after PORT or initiation of androgen deprivation therapy (ADT) for increasing PSA regardless of its value.RESULTS:
Ten-year biochemical failure-free survival, clinical failure-free survival, distant metastasisfree survival, overall survival (OS), and cause-specific survival were 60.5%, 76.2%, 84.4%, 91.1%, and 96.6%, respectively, at a median of 84 months after PORT. Pre-PORT PSA ≤ 0.5 ng/ml and Gleason's score ≤ 7 predicted favorable clinical outcomes, with 10-year OS rates of 92.5% and 94.1%, respectively. The 10-year OS rate was 82.7% for patients with a PSA > 1.0 ng/mL and 86.0% for patients with a Gleason score of 8-10. The addition of longterm ADT (≥ 12 months) to PORT improved OS, particularly in those with a Gleason score of 8-10 or ≥ T3b.CONCLUSION:
Clinical outcomes of PORT in a Korean prostate cancer population were very similar to those in Western countries. Lower Gleason score and serum PSA level at the time of PORT were significantly associated with favorable outcomes. Addition of long-term ADT (≥ 12 months) to PORT should be considered, particularly in unfavorable risk patients with Gleason scores of 8-10 or ≥ T3b.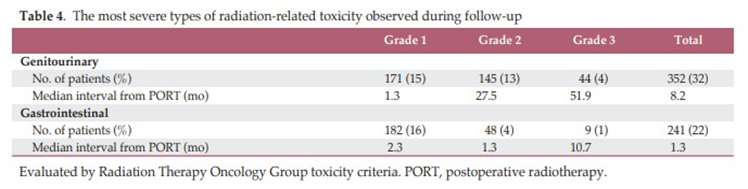
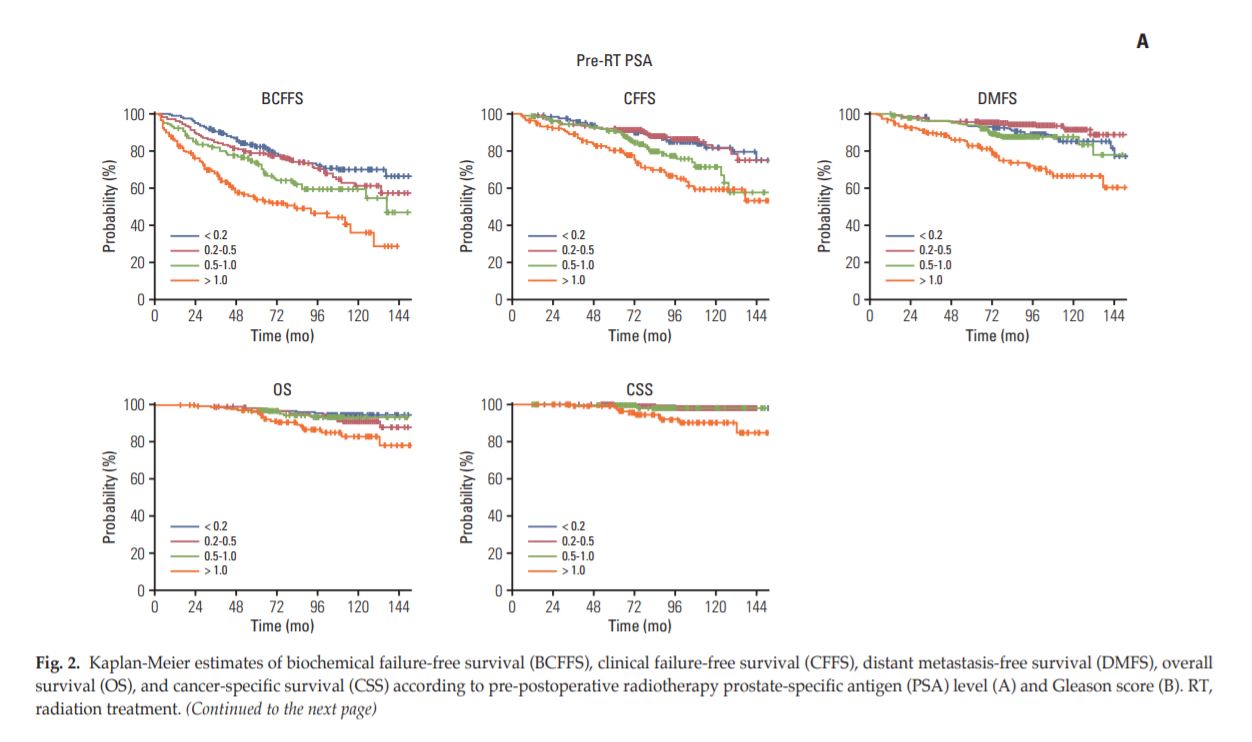
Fig A. 방사선치료 전 PSA 수치에 따른 biochemical failure-free survival, clinical failure-free survival, distant metastasis free survival, overall survival (OS) 과 cause-specific survival
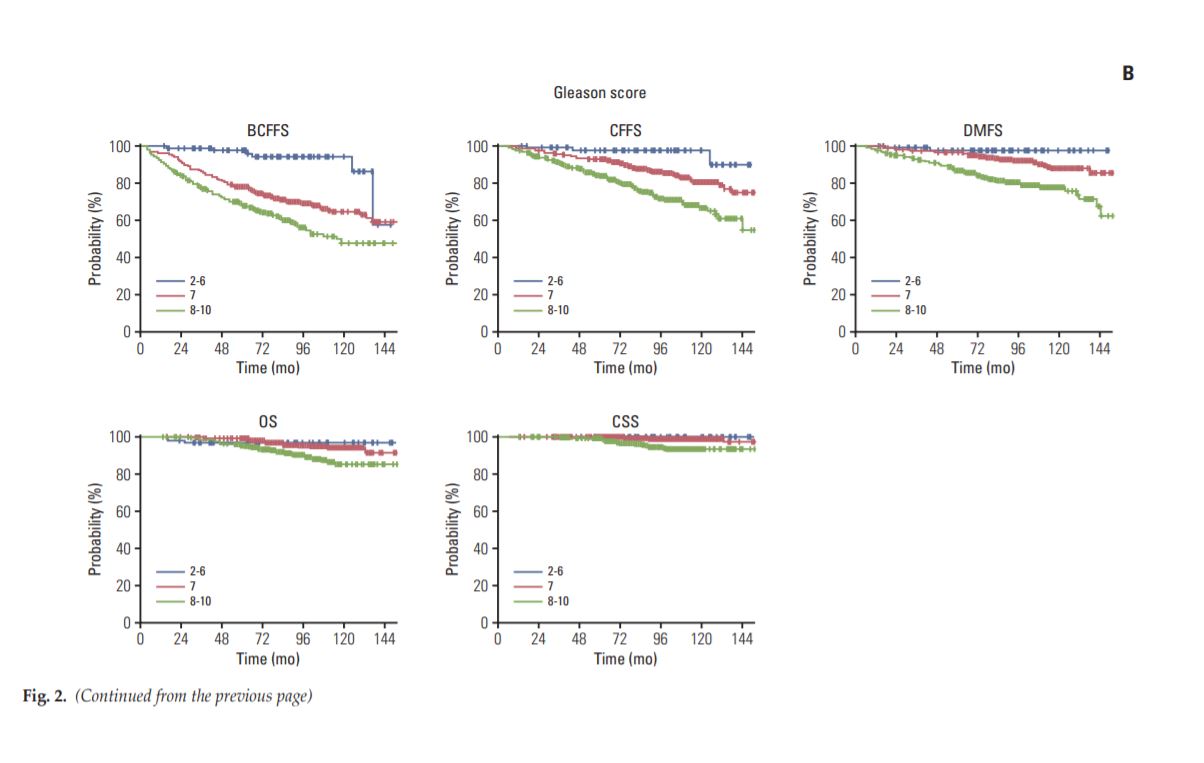
Fig B. Gleason’s score에 따른 biochemical failure-free survival, clinical failure-free survival, distant metastasis free survival, overall survival (OS) 과 cause-specific survival
Author informationLee SU1, Cho KH1, Park W2, Cho WK2, Kim JS3, Wee CW3, Kim YS4, Kim JH5, Nam TK6, Cho J7, Jeong SM8, Kim Y9, Shim SJ10, Choi Y11, Kim JS12.
1
The Proton Therapy Center, Research Institute and Hospital, National Cancer Center, Goyang, Korea.
2
Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
3
Department of Radiation Oncology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
4
Department of Radiation Oncology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
5
Department of Radiation Oncology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
6
Department of Radiation Oncology, Chonnam National University Hwasun Hospital, Chonnam National University College of Medicine, Hwasun, Korea.
7
Department of Radiation Oncology, Yonsei Cancer Center, Yonsei University College of Medicine, Seoul, Korea.
8
Department of Radiation Oncology, Ewha Womans University Medical Center, Ewha Womans University College of Medicine, Seoul, Korea.
9
Department of Radiation Oncology, Kyung Hee University Hospital, Kyung Hee University College of Medicine, Seoul, Korea.
10
Department of Radiation Oncology, Eulji Hospital, Eulji University School of Medicine, Seoul, Korea.
11
Department of Radiation Oncology, Dong-A University Hospital, Dong-A University School of Medicine, Busan, Korea.
12
Department of Radiation Oncology, Chungnam National University College of Medicine, Daejeon, Korea.
- 키워드
- Prostate-specific antigen; Prostatectomy; Prostatic neoplasms; Radiotherapy
- 연구소개
- 이 연구에서는 전립선암의 근치적 절제술을 받은 환자에 있어 수술 후 방사선치료의 장기적인 임상 결과와 예후인자를 분석하였습니다. 국내 19개 기관의 1000여명이 넘는 환자들을 포함하여 10년 성적을 분석한 귀중한 데이터라고 생각합니다. 10년 biochemical failure-free survival, clinical failure-free survival, distant metastasis free survival, overall survival (OS) 과 cause-specific survival 은 각각 60.5%, 76.2%, 84.4%, 91.1%, 96.6% 으로 평가 되었습니다. 예후 인자분석에서는 방사선치료 전 PSA 수치와 수술 당시 Gleason’s score가 전체생존율을 예측할 수 있는 중요한 인자였습니다. 방사선치료 전 PSA 수치가 0.5 ng/ml 이하인 그룹의 예후가 0.5 ng/ml 초과인 그룹보다 유의하게 좋게 관찰되었습니다. 또한 수술 당시 T병기가 높거나 (T3b이상), Gleason’s score가 8-10점 인 경우 호르몬 치료를 추가하는 것이 특히 도움이 되는 것으로 나타났습니다. 결론적으로 전립선암의 수술 후 방사선 치료 후 장기생존율이 90%이상 됨을 증명하였고, 의미있는 예후인자를 발굴함으로서, 임상영역에 도움을 줄 수 있는 연구 결과라고 생각합니다.
- 덧글달기
- 이전글 [In Vivo.] Reducing Radiation Dermatitis Using a Film-forming Silicone Gel During Breast Radiotherapy: A Pilot Randomized-controlled Trial.
- 다음글 [Radiother Oncol.] Combined transarterial chemoembolization and radiotherapy as a first-line treatment for hepatocellular carcinoma with macroscopic vascular invasion: Necessity to subclassify Barcelona Clinic Liver Cancer stage C.








편집위원
후향적 연구이지만 1,117명의 수술 후 방사선치료를 받은 전립선암 환자를 대상으로 생존율 및 부작용을 보고한 국내 다기관 연구로 서구와 비교할만한 성적과 함께 4%와 1%에서 grade 3의 late GU/GI toxcity가 발생하였다는 결과는 임상진료시 참고할만한 근거논문입니다.
2020-03-02 16:38:27