글로벌 연구동향
방사선종양학
- [Cancer Res Treat.] 코인두암 환자의 치료결과에 대한 의료기관 환자수 영향 : 다기관 후향적 분석 (KROG-1106)The Effect of Hospital Case Volume on Clinical Outcomes in Patients with Nasopharyngeal Carcinoma: A Multi-institutional Retrospective Analysis (KROG-1106).
국립암센터 / 하보람, 조관호*
- 출처
- Cancer Res Treat.
- 등재일
- 2019 Jan
- 저널이슈번호
- 51(1):12-23. doi: 10.4143/crt.2017.273. Epub 2018 Feb 5.
- 내용
Abstract
PURPOSE:
The purpose of this study was to investigate the effect of hospital case volume on clinical outcomes in patients with nasopharyngeal carcinoma (NPC).Materials and Methods:
Data on 1,073 patients with cT1-4N0-3M0 NPC were collected from a multi-institutional retrospective database (KROG 11-06). All patients received definitive radiotherapy (RT) either with three-dimensional-conformal RT (3D-CRT) (n=576) or intensity-modulated RT (IMRT) (n=497). The patients were divided into two groups treated at high volume institution (HVI) (n=750) and low volume institution (LVI) (n=323), defined as patient volume ≥ 10 (median, 13; range, 10 to 18) and < 10 patients per year (median, 3; range, 2 to 6), respectively. Endpoints were overall survival (OS) and loco-regional progression-free survival (LRPFS).RESULTS:
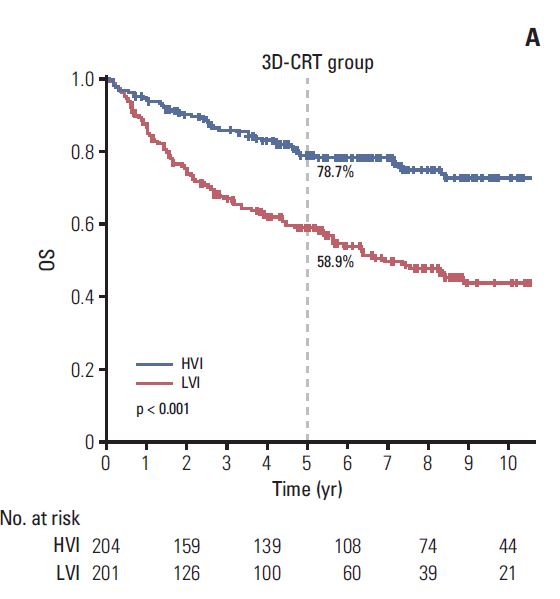
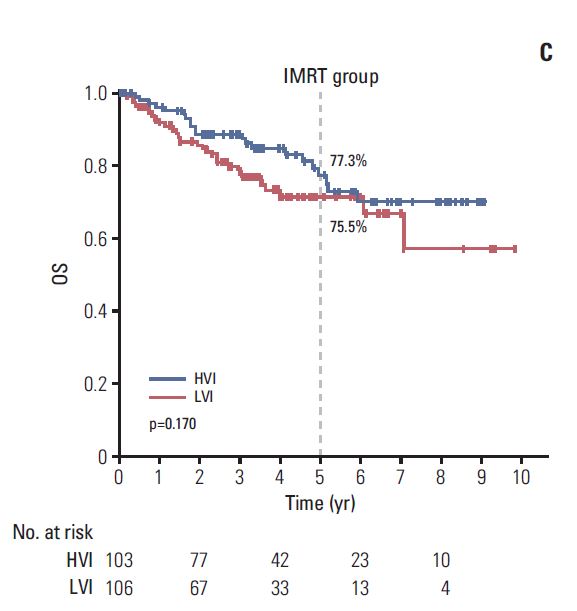
At a median follow-up of 56.7 months, the outcomes were significantly better in those treated at HVI than at LVI. For the 614 patients of propensity score-matched cohort, 5-year OS and LRPFS were consistently higher in the HVI group than in the LVI group (OS: 78.4% vs. 62.7%, p < 0.001; LRPFS: 86.2% vs. 65.8%, p < 0.001, respectively). According to RT modality, significant difference in 5-year OS was observed in patients receiving 3D-CRT (78.7% for HVI vs. 58.9% for LVI, p < 0.001) and not in those receiving IMRT (77.3% for HVI vs. 75.5% for LVI, p=0.170).CONCLUSION:
A significant relationship was observed between HVI and LVI for the clinical outcomes of patients with NPC. However, the difference in outcome becomes insignificant in the IMRT era, probably due to the standardization of practice by education.
Author informationHa B1, Cho KH1, Moon SH1, Lee CG2, Keum KC2, Kim YS3, Wu HG4, Kim JH4, Ahn YC5, Oh D5, Noh JM5, Lee JH6, Kim SH6, Kim WT7, Oh YT8, Kang MK9, Kim JH10, Kim JY11, Cho MJ12, Kay CS13, Choi JH14.
1
Proton Therapy Center, Research Institute and Hospital, National Cancer Center, Goyang, Korea.
2
Department of Radiation Oncology, Yonsei University College of Medicine, Seoul, Korea.
3
Department of Radiation Oncology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
4
Department of Radiation Oncology, Seoul National University College of Medicine, Seoul, Korea.
5
Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
6
Department of Radiation Oncology, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea.
7
Department of Radiation Oncology, Pusan National University Hospital, Busan, Korea.
8
Department of Radiation Oncology, Ajou University School of Medicine, Suwon, Korea.
9
Department of Radiation Oncology, School of Medicine, Kyungpook National University, Daegu, Korea.
10
Department of Radiation Oncology, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea.
11
Department of Radiation Oncology, Yeouido St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
12
Department of Radiation Oncology, Chungnam National University School of Medicine, Daejeon, Korea.
13
Department of Radiation Oncology, Incheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea.
14
Department of Radiation Oncology, Chung-Ang University Hospital, Seoul, Korea.
- 키워드
- Hospital; Intensity-modulated radiotherapy; Low- or high-volume; Nasopharyngeal neoplasms; Three-dimensional conformal radiotherapy; Treatment outcome
- 연구소개
- 이 논문은 대한방사선종양학임상연구회(KROG-1106)에 등록된 근치적 방사선치료를 받은 1073명의 비인강암(T1-4N0-3M0) 환자를 대상으로 hospital case volume에 따른 치료결과를 분석한 후향적 연구입니다. Propensity score matching 후, 연간 10명 이상 치료한 HVI (high volume institution)과 10명 미만을 치료한 LVI (low volume institution)으로 구분하였을 때, 5년 생존율이 78.4% vs. 62.7% (p=<0.001) 로 HVI에서 높았습니다. 이 같은 차이는 삼차원입체조형치료 시 78.7% vs. 58.9% (p <0.001)로 차이가 뚜렷했으나, 세기조절방사선치료 시에는 77.3% vs. 75.5% (p=0.170)로 별 차이가 없었습니다. 이는 세기조절방사선치료 도입 시, 표준화된 target drawing, 컴퓨터 플랜 등, 교육으로 인해 LVI의 치료 결과가 상향평준화 된 것으로 생각됩니다. 이 같은 현상은 여러 암 수술 치료에서 이미 알려진 바로, 이 논문의 의의는 암의 방사선치료에서도 유사한 결과를 확인하였다는 것이며, 더욱 고무적인 것은, 이 같은 차이는 교육으로 극복될 수 있다는 것입니다.
- 덧글달기








편집위원
다양한 암종에서 hospital volume에 따른 survival disparity는 여전히 관심의 대상이 되어오고 있으며, 치료기법에 따른 분석을 추가하여 의미있는 결론을 도출한 연구임
2019-02-22 16:41:17